For years, Medicare’s coverage of telehealth was limited. People in rural communities could access care but only if their services were completed at a Medicare-approved location. Surprisingly, you could be at a doctor’s office, clinic, hospital, mental health center, or skilled nursing facility but you would not be covered if you reached out to a provider from your home.
Thankfully, Medicare expanded its telehealth services in 2019. People on dialysis could begin to use telehealth from dialysis clinics or from their homes. Telehealth from home also became an option for people who had substance abuse and mental health disorders. Telestroke services from a hospital or mobile stroke unit were no longer restricted to rural areas. While these measures improved access to care, many people were still left without telehealth options.
The pandemic crisis moved the needle
The coronavirus pandemic changed everything. It became dangerous for people to sit in waiting rooms where they could be potentially exposed to the virus. People who had to quarantine after an exposure or who had an infection still needed care from healthcare providers, whether it was for COVID-19 or for other reasons. Did the risk of a real-life office visit outweigh the risk of not getting medical care?
In March 2020, the Centers of Medicare & Medicaid Services expanded Medicare services to make it easier for people to get the care they needed. Instead of limiting telehealth to people in rural communities or to people with certain medical conditions, all beneficiaries were able to use these services and could do so from the comfort of their own homes.
66% of our respondents used telehealth
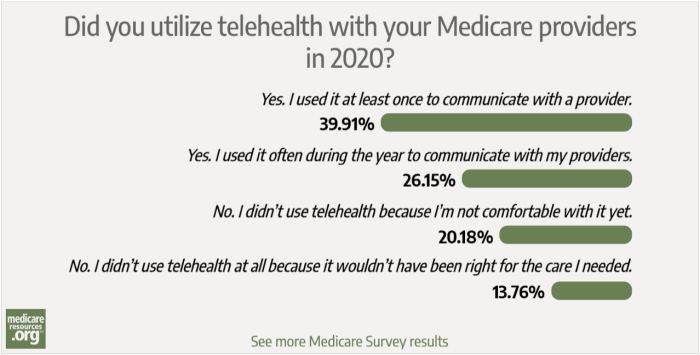
Given the aforementioned factors, we expected a growing number of Medicare enrollees to give telehealth a try. And, not surprisingly, our most recent poll did show a high percent of our readers (more than 200 responding) did use telehealth in 2020. We asked: “Did you utilize telehealth with your Medicare providers in 2020?”
The responses:
- 39.9% – Yes. I used it at least once to communicate with a provider.
- 26.2% – Yes. I used it often during the year to communicate with my providers.
- 20.2% – No. I didn’t use telehealth because I’m not comfortable with it yet.
- 13.8% – No. I didn’t use telehealth at all because it wouldn’t have been right for the care I needed.
I’ll talk more about why Medicare enrollee did utilize telehealth later, but first, here’s my take on why roughly a third of our respondents did not.
New and not always user-friendly technology
For the purposes of Medicare, telehealth is defined as two-way real-time video-conferencing between a beneficiary and a healthcare provider. A phone call, for example, would not typically count as a telehealth visit since it only has an audio component. During the public health crisis, however, CMS is allowing coverage for some phone services too. Time will tell if audio-only services will continue to be covered once the pandemic is over.
Telehealth requires users to have two types of technology: 1) internet connectivity and 2) the appropriate software for conferencing. Users can look to increasingly popular online tools like FaceTime, Skype, or Zoom to communicate with thier providers. (Users should keep in mind that telehealth software is most secure when it is certified as HIPAA compliant. Providers will let patients know the specific software program they’ll need to download but, in all cases, that software will be free to users.)
Generally speaking, this type of software tends to be straightforward and easy to use, though you may need some guidance to set it up the first time.
That said, confusion – and perhaps mistrust about that technology – may explain why 20% of our respondents didn’t use telehealth services in 2020.
Some people may simply not feel comfortable using new technology and may be hesitant to give it a try. For others willing to try, there may be a learning curve (which could explain why about 40% of our respondents used at least once but not often).
Others patients may have concerns about internet security or that the software could be “hacked.” In my experience, mistrust about this technology is generally unfounded. HIPAA compliance is taken very seriously. Failure to protect your information could lead to high fines and penalties for your provider and/or the software companies they use. Be assured that your provider is taking every precaution to protect you.
Concerns that telehealth won’t help
Another misconception about telehealth is that it won’t cover what you need. The 14% of readers in this survey that said “it wouldn’t have been right for the care I needed” may truly have had conditions that were not appropriate for telehealth – but it’s also possible a portion of them likely could have benefited from those services.
When many people think of office visits, they think of the laying-on of hands. A doctor may listen to your heart and lungs with a stethoscope. They may perform tests on your blood, saliva, or urine. It would seem that your provider would be limited in what they can do over a screen.
That is true to an extent but you may be surprised how much information can be gleaned during a telehealth visit. With the proper lighting, your healthcare provider can assess rashes and other skin conditions. They might even be able to get a good look in your throat. When concerns are raised about stroke, a doctor can look for facial asymmetry and other neurological findings by asking you to do certain maneuvers.
Let’s not forget that many people have thermometers at home. In light of the pandemic, many may even have pulse oximeters to check their oxygen levels. Depending on their underlying health conditions, they may also have other tools like blood pressure cuffs and glucometers to check their blood sugar.
The discussion with your provider is key
Still, the most important part of any doctor visit is the discussion. In a telehealth visit, a provider can still frequently make a diagnosis based on your history. When needed, they can send orders to a laboratory or send prescriptions directly to your pharmacy through the electronic medical record.
If your provider sees that there is an issue that needs more urgent or hands-on attention, they could advise you to come into their office (if they are open) or advise you to go the emergency room.
Examples of services covered by Medicare telehealth services include but are not limited to:
- Acute stroke services
- Annual wellness visits
- Behavioral counseling
- Chronic disease follow-ups
- Dialysis education and management
- General consultations
- Hospital follow-ups
- Medication management
- Mental health screening
- Obesity counseling
- Physical therapy, occupational therapy, and/or speech therapy sessions
- Psychotherapy
- Sick visits
- Smoking cessation sessions
- Substance abuse screening and counseling
Why telehealth makes sense
The ability to access care from home for such a wide range of services is convenient. Better yet, it is a cheaper and safer option than going into the office.
With the exception of Annual Wellness Visits and other preventive screening services which are free, Medicare patients typically pay 20% cost-sharing for each doctor visit. During the pandemic, however, CMS is allowing providers to waive that cost-sharing so that these telehealth services may be free to you.
National utilization of telehealth
The Centers for Disease Control and Prevention reported a 154% increase in overall telehealth use in the last week of March 2020 compared with the same week in 2019. A study in Health Affairs, focused on Medicare beneficiaries, found that approximately 13,000 Medicare beneficiaries received care in the weeks prior to the pandemic but the number skyrocketed to 1.7 million per week after CMS expanded telehealth coverage. It seems many of our readers have followed suit.
Whether you have chronic conditions that require regular check-ups or you have a new health concern, do not hesitate to reach out to your provider. Even if you are not able to see them in person, a telehealth visit may be just what the doctor ordered.
Tanya Feke M.D. is a licensed, board-certified family physician. As a practicing primary care physician and an urgent care physician for nearly ten years, she saw first-hand how Medicare impacted her patients. In recent years, her career path has shifted to consultant work with a focus on utilization review and medical necessity compliance.
Dr. Feke is an expert in the field, having Medicare experience on the frontlines with both patients and hospital systems. To educate the public about ongoing issues with the program, she authored Medicare Essentials: A Physician Insider Reveals the Fine Print. She has been frequently referenced as a Medicare expert in the media and is a contributor to multiple online publications. As founder of Diagnosis Life, LLC, she also posts regular content about health and wellness to her site at diagnosislife.com.