Medicare Advantage open enrollment period
Starting in 2019, the Cures Act created an annual Medicare Advantage open enrollment period – from January through March – when Medicare Advantage enrollees can choose a different Advantage plan or switch to Original Medicare with or without a separate Medicare Part D plan. The Medicare Advantage open enrollment period replaced the Medicare Advantage disenrollment period, which was created by the Affordable Care Act and existed from 2011 to 2018.
Medicare Advantage disenrollment lasted for only the first 45 days of each year, as opposed to the first three months for the Medicare Advantage open enrollment period. Medicare Advantage disenrollment allowed Advantage plan members to switch to Original Medicare and choose a stand-alone Part D plan if they wished, but could not be used to change from one Advantage plan to another. So the new window is longer and more flexible than the old one. But enrollees are limited to a single change during Medicare Advantage open enrollment, as opposed to multiple changes during Medicare’s fall open enrollment.
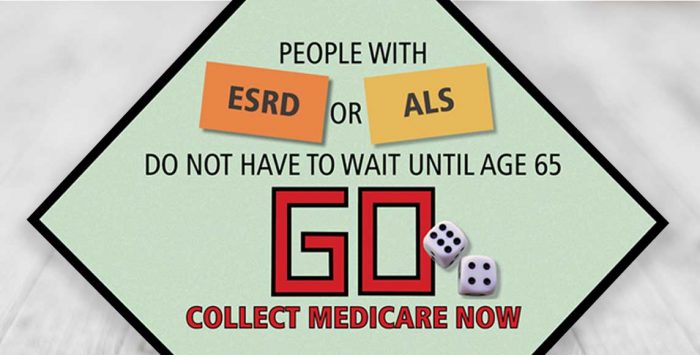
People with ESRD allowed to enroll in Medicare Advantage as of 2021
The Cures Act also expanded who can enroll in Medicare Advantage. While most Medicare beneficiaries have an array of coverage options, individuals with End Stage Renal Disease (ESRD) – also known as kidney failure – face fewer choices and potentially large out-of-pocket costs due to the expensive nature of kidney dialysis. Americans with ESRD have historically been unable to enroll in Medicare Advantage plans other than the ESRD chronic condition Special Needs Medicare Advantage plans (C-SNPs) available in few areas. (However, people diagnosed with ESRD after enrolling in an Advantage plan are allowed to retain that coverage.)
An ESRD diagnosis triggers Medicare eligibility, regardless of the person’s age. But the only option for most ESRD beneficiaries is Original Medicare, with potentially high out-of-pocket costs (beneficiaries pay an uncapped 20 percent coinsurance for Part B services, including dialysis). Compounding this issue, there is no federally mandated period when people under 65 can buy Medigap plans on a guaranteed issue basis, without medical underwriting. Some states have kept their high-risk pools open to individuals in this situation, and quite a few states have implemented rules to ensure access to Medigap plans for people under age 65. But some of those states still exclude people with ESRD from those protections (click on a state on this map to see how Medigap rules work for people under age 65).
The good news for people with ESRD is the Cures Act changed the law so people with kidney failure will be able to enroll in Medicare Advantage starting in 2021. While Advantage plans can have high out-of-pocket maximums – $6,700 is the federal limit in 2020, with plans averaging around $5,000 – this is better than not having any protection against out-of-pocket costs.
Tags: 21st Century Cures Act, legislation, Medicare Advantage, Medicare open enrollment, open enrollment